Advanced Solutions
for Advanced Pathology
Parathyroid Hormone (PTH) (MRQ-31)
Mouse Monoclonal Antibody
Cat. No. Description
Volume
45249 IMPATH PTH RTU M (MRQ-31)
50 Tests
44363 PTH RTU M (MRQ-31)
7 ml Ready To Use
44746 PTH 0,1 M (MRQ-31)
100 µl liquid Concentrated
44747 PTH 1 M (MRQ-31)
1 ml liquid Concentrated
Product Specifications
Designation
IVD
Reactivity
Paraffin
Visualization
Cytoplasmic, Membranous
Control
Parathyroid Tissue
Stability
Up to 36 mo. at 2-8°C
Isotype
IgG
2a
Manual Protocol*
• Pretreatment: Heat Induced Epitope
Retrieval (HIER)
• Primary Antibody Incubation Time:
10-30min @ 25-37°C
• 2-step polymer detection
*Please refer to product insert for complete protocol.
ImPath Protocol*
• Dewax: Dewax Solution 2 (DS2)
• Pretreatment: Retrieval Solution pH 9.0
(TR1) 32min @ 98-103°C
• Primary Antibody Incubation Time:
10-90min @ 25-37°C
• HRP Polymer (Universal) or AP Polymer
(Universal) for 12 min
*Please refer to product insert for complete protocol.
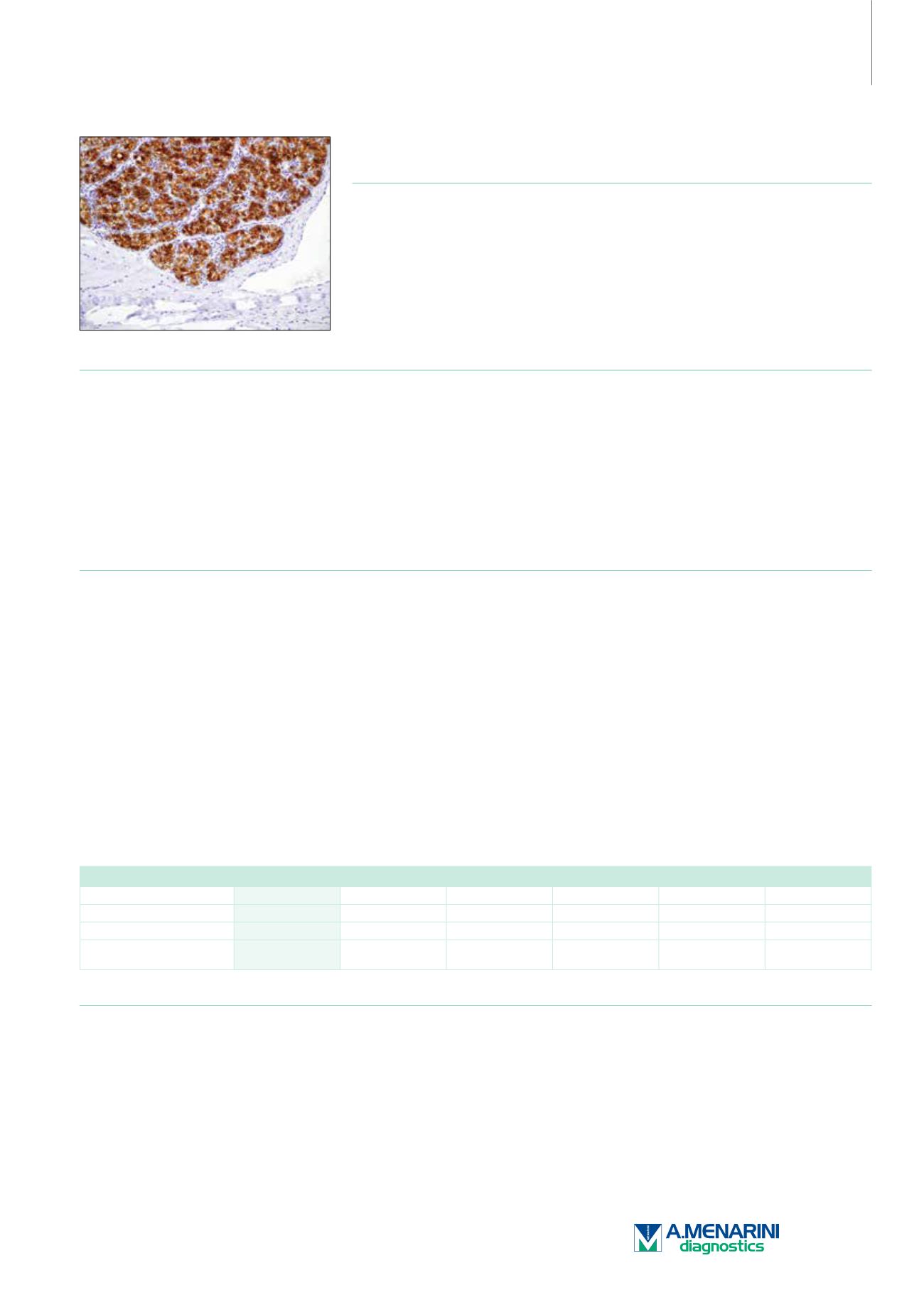
Product Description
Surgical pathologists are familiar with the ability of parathyroid proliferations to assume a variety of histological guises, posing difficulty to
categorize any given lesion as hyperplastic, adenomatous, or carcinomatous in nature. This is usually resolved with macroscopic appearance of
the remaining parathyroid glands as assessed by the surgeon. The role of the surgical pathologist is to identify the lesion as parathyroid in nature
and to assess whether it is normocellular or hypercellular. Although easily accomplished in the majority of instances, rare examples of parathyroid
hyperplasia/adenoma showing a follicular/trabecular arrangement may cause concern over the alternative diagnosis of a thyroid adenoma.
This becomes more pertinent when the parathyroid lesion abuts into the thyroid gland or lies within the thyroid capsule. Immunostaining for
thyroglobulin and parathyroid hormone (PTH) is especially useful to resolve the problem.
Anti-PTH antibody is also useful to distinguish parathyroid hyperplasia/neoplasms from thyroid and metastatic neoplasms although the
pathologist is typically aware of the preoperative hypercalcemic status. Occasionally when the surgeon does not supply this information, PTH
immunohistochemistry is essential. Even more problematic are situations in which clear cell parathyroid carcinomas are nonsecretory without
an abnormality in mineral metabolism. In such situations, metastatic renal cell carcinoma or metastatic clear cell carcinoma of the lung is
evident warranting PTH immunohistochemistry to arrive at the correct diagnosis. The other instance in which PTH antibodies are useful is in the
consideration of parathyroid carcinomas located primarily in the anterior mediastinum (intrathymically). In this situation, distinction from primary
thymic metastatic carcinomas, non-Hodgkin lymphoma, and germ cell tumors is necessary.
Differential Diagnosis of Parathyroid Tumors
PTH
Chromogranin A Synaptophysin
S-100
TTF-1
Calcitonin
Parathyroid Tumors
+
+
+
-
-
-
Follicular Cell Tumors
-
-
-
+/-
+
-
Medullary Thyroid
Carcinoma
-
+
+
-
+
+
Reference
1. Aldinger KA, et al. Cancer. 1982; 49:388-97.
2. Brown EM. Mineral Electrolyte Metal. 1982; 8:130-50.
3. Chen HL, et al. Journal of Biology and Chemistry. 2002; 277:19374-81.
4. Habener JF, et al. Physiology Reviews. 1984; 64:985-1053.
5. Murphy MN, et al. Cancer. 1986; 58:2468-76.
6. Permanetter W, et al. American Journal of Surgical Pathology. 1983; 7:535-46.
7. Wick MR, et al. Seminars in Diagnostic Pathology. 1997; 14:183-202.
193